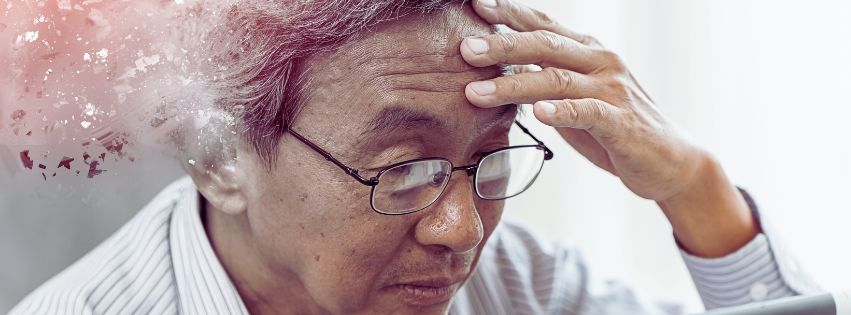
Understanding the Link Between Gum Disease and Alzheimer’s: Exploring the Oral Health Connection
Research has indicated a correlation between gum disease and Alzheimer’s, suggesting that individuals with gum disease may experience a significantly faster decline in memory. For instance, one study observed that memory decline was six times faster in those with gum disease over a six-month period. This suggests that gum disease could potentially accelerate cognitive decline in Alzheimer’s, possibly due to inflammatory reactions within the body.
Is There a Connection Between Gum Health and Alzheimer’s?
According to Dioguardi, gum disease is associated with elevated levels of pro-inflammatory molecules in the bloodstream. This chronic inflammation can trigger ongoing inflammation in the brain, known as neuroinflammation, leading to nerve cell deterioration and contributing to Alzheimer’s disease. While direct causation hasn’t been definitively established, current studies indicate a connection between gum disease and Alzheimer’s through common pathways of inflammation. Maintaining regular dental hygiene practices may potentially reduce the associated risks.
Can Periodontal Disease Contribute to Alzheimer’s Development?
Periodontitis, a chronic inflammation affecting the tissues surrounding teeth, is considered a potential risk factor for Alzheimer’s disease (AD). It results from complex bacterial interactions, leading to the breakdown of supportive structures around teeth. Recent evidence suggests a possible connection between periodontal (gum) disease and Alzheimer’s. Periodontal disease involves persistent inflammation and bacterial infections in the gums, often resulting in tissue damage and tooth loss if untreated. Alzheimer’s, on the other hand, is characterized by the accumulation of amyloid plaques and neurofibrillary tangles in the brain, causing neurodegeneration.
Researchers propose that the chronic inflammation and bacterial presence in periodontal disease could contribute to Alzheimer’s development or progression through various mechanisms, including systemic inflammation, bacterial spread, and immune responses impacting the brain. Studies indicate that individuals with periodontal disease are more prone to cognitive impairment and Alzheimer’s compared to those with healthy gums. Additionally, certain bacteria linked to periodontal disease have been discovered in the brains of Alzheimer’s patients, suggesting a potential pathway for bacterial migration from the mouth to the brain.
While this association is intriguing, it’s crucial to note that definitive causation has not been established. Factors such as genetics, lifestyle, and other health conditions also influence Alzheimer’s risk. Nevertheless, maintaining good oral hygiene and promptly treating gum disease may have broader health implications, potentially reducing the risk of Alzheimer’s and other systemic conditions. Further research is essential to fully grasp the intricate relationship between periodontal disease and Alzheimer’s.
Does Flossing Prevent Alzheimer’s?
Recent research exploring the connection between oral health and dementia suggests a speculative possibility for reducing dementia risk by addressing oral bacteria. A study conducted in the United States revealed that individuals with gum disease and mouth infections were more prone to developing Alzheimer’s, the leading cause of dementia.
While flossing is known to promote overall oral hygiene, there is currently no direct evidence suggesting it prevents Alzheimer’s. However, maintaining good oral hygiene practices, including regular flossing, might help lower the risk of gum disease, which has been tentatively associated with Alzheimer’s. By reducing inflammation and bacterial presence in the mouth, consistent flossing could indirectly support brain health. Nonetheless, further research is necessary to determine the exact impact of oral hygiene habits, such as flossing, on preventing Alzheimer’s disease.
Which Specific Bacteria in the Mouth are Linked to Alzheimer’s Disease?
Researchers have discovered that a particular type of bacteria, known as Porphyromonas gingivalis, has the ability to travel from the mouth to the brain. Once it reaches the brain, this bacteria releases enzymes called gingipains, which can damage nerve cells. This damage may contribute to memory loss and the development of Alzheimer’s disease over time.
Several specific oral bacteria have been implicated in Alzheimer’s disease, including Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia, which are commonly associated with gum disease. These bacteria produce toxins and trigger inflammation in the gums, potentially leading to systemic inflammation and the spread of bacteria throughout the body, including the brain.
Porphyromonas gingivalis, in particular, has attracted attention for its role in Alzheimer’s disease. This bacterium’s gingipains can breach the blood-brain barrier, facilitating the formation of amyloid plaques and neurofibrillary tangles, which are characteristic features of Alzheimer’s pathology. Studies have also detected increased levels of Porphyromonas gingivalis DNA in the brains of Alzheimer’s patients, suggesting its potential contribution to the progression of the disease.
Although these findings imply a connection between oral bacteria and Alzheimer’s, further research is needed to fully understand the mechanisms involved and to investigate potential therapeutic strategies targeting oral microbial populations for the prevention or treatment of Alzheimer’s disease.
What is the Link Between Gum Disease and Alzheimer’s?
An oral health issue associated with Alzheimer’s is periodontal disease, characterized by chronic inflammation affecting the supportive tissues of the teeth. This condition arises when the gums become infected due to the accumulation of plaque and tartar.
The link between Alzheimer’s and teeth lies primarily in oral health. Research suggests that poor oral hygiene and certain oral conditions, such as gum disease, may increase the risk of Alzheimer’s disease. Chronic inflammation and bacterial infections in the mouth, particularly from periodontal disease, can lead to systemic inflammation, potentially affecting the brain. Additionally, specific oral bacteria, such as Porphyromonas gingivalis, have been implicated in Alzheimer’s pathology, with evidence of their presence in the brains of affected individuals. Maintaining good oral hygiene practices, including regular brushing, flossing, and dental check-ups, may help reduce the risk of gum disease and potentially lower the risk of Alzheimer’s disease by minimizing inflammation and bacterial exposure.